



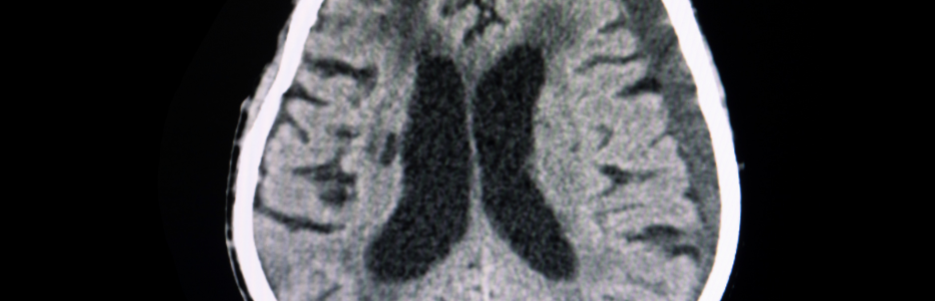
A Subdural Hematoma (SDH) is a collection of blood between the dura mater (the outer layer of the meninges) and the brain. It occurs when blood vessels, typically veins, rupture and bleed into the subdural space.

Most severe and life-threatening type.
Develops rapidly after a head injury.
Blood collects quickly, causing increased pressure on the brain.
Requires immediate surgical intervention.

Develops over days to weeks after an injury.
Symptoms may be gradual but worsen over time.
May require surgical or conservative management, depending on severity.

Develops slowly over weeks or months, often without a major injury.
More common in elderly individuals or those on blood thinners.
Symptoms are subtle at first (confusion, memory issues).
Treatment may involve monitoring or drainage procedures.
The symptoms depend on the size and location of the hematoma and the rate of bleeding:
in arms or legs
(in severe cases)
Individuals with the following risk factors are more prone to developing SDH:

SDH is primarily caused by:
Falls, car accidents, or sports injuries.
Sudden impact causes vein rupture.
Especially in the elderly, minor trauma can still cause SDH.
Symptoms may appear days or weeks later.
Occurs without head trauma.
Common in people on blood thinners.
Seen in older adults, where the brain shrinks slightly.
Creates more space between the brain and skull, making veins prone to rupture
While not all SDH cases are preventable, you can reduce the risk by:
Use handrails and non-slip mats at home.
Wear protective gear during sports or activities.
Regular exercise to improve balance.
Seat belts and airbags in vehicles.
Helmets for cycling, motorbiking, and sports
Regular monitoring of INR levels if on anticoagulants.
Consult a doctor before taking blood-thinning medications.
Limit alcohol consumption, as it increases fall risk.
Seek help for alcohol abuse
Manage hypertension and clotting disorders to reduce bleeding risk.
Regular medical checkups for at-risk individuals.
In mild cases, non-surgical treatments may suffice:
Small or stable SDH may not require surgery.
CT scans monitor size and progression.
Neurological exams track symptoms.
Pain relievers (acetaminophen) for headaches.
Anticonvulsants to prevent seizures.
Osmotic diuretics (mannitol) to reduce brain swelling.
Bed rest and hydration.
Frequent monitoring for neurological changes.


Minimally invasive procedure.
Small holes are drilled into the skull.
Blood is drained using suction or irrigation.
Used for chronic SDH or smaller hematomas.
Recovery: 1–2 days in the hospital.

Open brain surgery for larger hematomas.
Bone flap is removed to access and drain the hematoma.
The flap is replaced after bleeding control.
Used for acute SDH.
Recovery: 4–6 weeks.

More extensive surgery than a craniotomy.
Bone flap is removed and not immediately replaced.
Used in cases of severe brain swelling.
Bone flap may be replaced later.
Recovery: Longer and more complex.

Minimally invasive technique.
Endoscope is inserted through a small opening.
Used for chronic or subacute SDH.
Shorter recovery time.

2–7 days, depending on severity.
4–12 weeks, with gradual improvement.
Avoid strenuous activities.
Frequent follow-up scans (CT or MRI).
Monitor for neurological changes.
Physical therapy if mobility is affected.

Reduces brain pressure and prevents permanent damage.
Improves neurological function.
Prevents complications like seizures and brain herniation.
Enhances quality of life.