



These surgeries are performed when the valves become too narrow (stenosis) or leaky (regurgitation), affecting heart function and blood circulation.

Made of durable materials (metal, carbon, plastic), requiring lifelong blood thinners.

Made from human or animal tissue, lasts 10–20 years but does not require lifelong blood thinners.

A minimally invasive alternative for high-risk patients needing AVR.

Uses small incisions for quicker recovery.

The patient’s pulmonary valve replaces the aortic valve.
Patients may experience:
(especially during activity)
Although valve replacement surgery is often successful, risks include:

These surgeries are required due to:
Congenital heart defects (born with valve abnormalities)
Rheumatic heart disease (caused by untreated strep throat infections)
Aging and calcification (valves stiffen over time)
Heart infections (endocarditis)
Heart attacks affecting valve function
Aortic aneurysm (enlargement of the aorta affecting the aortic valve)
While some valve conditions are unavoidable, you can lower risks by:
Before recommending valve replacement, doctors may try:
Blood thinners, beta-blockers, diuretics to manage symptoms.
A catheter-based procedure to open a narrowed valve (used mostly for mitral stenosis).
Diet, exercise, weight management.

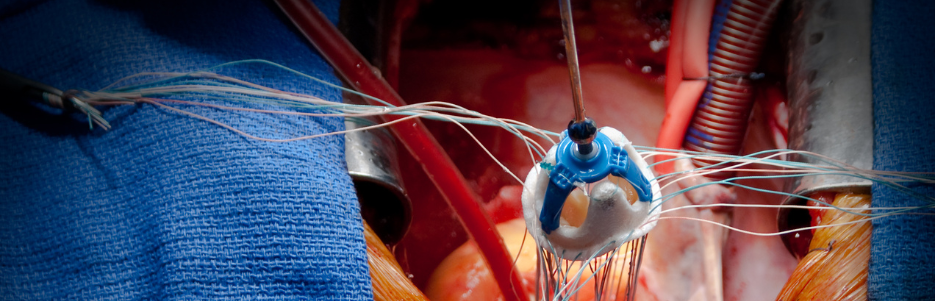
Open-Heart Valve Replacement – The chest is opened to replace the damaged valve.
Minimally Invasive Valve Surgery (MIVS) – Small incisions are used instead of a full chest opening.
Transcatheter Aortic Valve Replacement (TAVR/TAVI) – A catheter-based procedure for high-risk patients needing AVR.
Percutaneous Mitral Valve Repair (MitraClip) – A catheter-based option for high-risk MVR patients.
Ross Procedure – The patient’s pulmonary valve replaces the aortic valve.

Hospital Stay – Usually 5–7 days.
Full Recovery – Takes 6–12 weeks, depending on the procedure.
Lifelong Monitoring – Patients may require blood thinners (for mechanical valves).
Cardiac Rehabilitation – Exercise and diet programs to improve heart health.